Blog
Tanzanian Healthcare, Part II: A day in the life of an internist at Dareda

Tanzanian Healthcare, Part II: A day in the life of an internist at Dareda
February 19, 2018
The morning after I arrived, there was a gentle knock at my door. A young nun dressed in a religious habit introduced herself as Sister A. She informed me that she will be hosting me during my stay at Dareda. She is an internal medicine trained specialist at the hospital. After a few minutes of pleasantries, I asked her an obvious question. “Are you from India?” She smiled widely and said yes – from Kerala. As it turns out, she is from the same district as my family. In fact, she was familiar with my parents’ family names. In Kerala, your family name, or house name, is the main identifier as opposed to your last name. I semi-jokingly told her I’m sure we are related in some way.
Sister A., sometimes called Dr. A. or Sister Dr. A. by hospital staff, joined the convent at the age of 16 and is now a member of the Adoration Sisters congregation. At 21, when the opportunity to serve in Tanzania arose, she accepted. She completed medical school, internship and residency in Tanzania. It’s the relaxed culture and strong personal and professional relationships that she appreciates here.
On my first Monday morning, I spent several hours with Sister A. We attended mass first thing in the morning, a requirement for all hospital leaders (my mom will be thrilled to hear this), followed by morning report, a meeting of the clinical staff to hear the overnight report on patients and have clinical discussions on notable cases. After morning report, Sister A., Dr. L, the Medical Officer in Charge and I dove right into a discussion on international politics and challenges in health care over a simple breakfast of chapatis and coffee in the hospital canteen. The role of Medical Officer in Charge is equal to that of Medical Director in the US.
The greatest needs, they explained, are basic diagnostic equipment and specialty-trained physicians. They lack specialty-trained physicians such as general surgeons, pediatricians, orthopedic surgeons and OB/GYNs, to name a few. Of note is that 68% of their inpatient population is maternal child and pediatrics. The providers receive as much training as possible from courses and visiting specialists to provide these services to patients. Once they reach their limits, they transfer patients out to higher level facilities.
Here, an “MD” refers to a physician who completed medical school and one year of internship. A “specialist” is a physician who completed residency training in a particular specialty. Sister A. is the only specialist at Dareda Hospital. Next week, she leaves to spend 2 months at my former employer in the Bronx to refine her endoscopy skills. Thanks to their generosity, the hospital now has two endoscopes. She and the Dr. L. were both trained in adult endoscopy. She is hoping to refine her skills to train more providers and expand the service to more patients.
As the conversation continued about resources, Sister A. described a forty-seven year old patient of hers admitted for a presumed blood clot in his lungs, known as pulmonary embolism. He developed a serious condition called cardiogenic shock and was in critical condition. In the US, this patient would have been on a ventilator in an ICU. At Dareda, there are no critical care resources. After weighing her options, she thought of one last resort to save his life. She started the patient on an IV adrenaline drip. It worked. His blood pressure rose and he began to recover. After breakfast, we rounded on him. He was awake, alert and recovering. Sadly, I learned this week that he deteriorated. His prognosis became grim again.
Next, we rounded on a new patient admitted to the female ward, a thirty-seven year old known diabetic brought in by a relative for vomiting, abdominal pain and confusion. Her blood sugar was over five times the normal limit causing a condition known as diabetic ketoacidosis (DKA). On rounds, she was completely unresponsive, her limbs flaccid and cold and her breathing labored. I asked about her blood chemistries, a standard test that’s arguably over ordered in US hospitals. “We don’t have the equipment for chemistries here.”, she replied. She elicited the patient’s medical history from the family member and diligently performed a physical exam. She concluded that the patient was also in shock, but this one was due to infection of unknown source. She wrote resuscitation orders in the hopes of saving her. There was really no other option as she was too unstable for transfer to another hospital. She was unsure if she would survive. The next day I learned that she had markedly improved.
As I toured the hospital, the lack of basic resources described was quickly validated. I marveled at how Sister A. and the clinical teams took care of their patients without the basic diagnostic equipment and medications on which we rely heavily in the US. It calls into question how much we do that is truly unnecessary. Every patient that enters an emergency department gets a battery of diagnostic tests. Once admitted, this increases exponentially. It’s well known in the medical community that much of the information needed to make a diagnoses can be elicited from a good history and physical exam. But yet just having these resources at our disposal encourages over-utilization resulting in a tremendous amount of waste. The reasons are complex. On the flip side, clinicians at Dareda are crippled without basic clinical resources and overly reliant on history and physical exam. In the end, neither produce better health outcomes.
While there is no obvious solution, one thing is clear. Health care systems that optimize resource use with the goal of ensuring better outcomes would serve us all better, regardless of what side of the globe we are on.
Stay tuned for Part III in this series where I will share more on the economics of providing care at Dareda.
Discover more from diannajacob.com
Subscribe to get the latest posts sent to your email.
Recent News

About Dianna
May 29, 2024

On Being Single and Child-Free
July 31, 2022
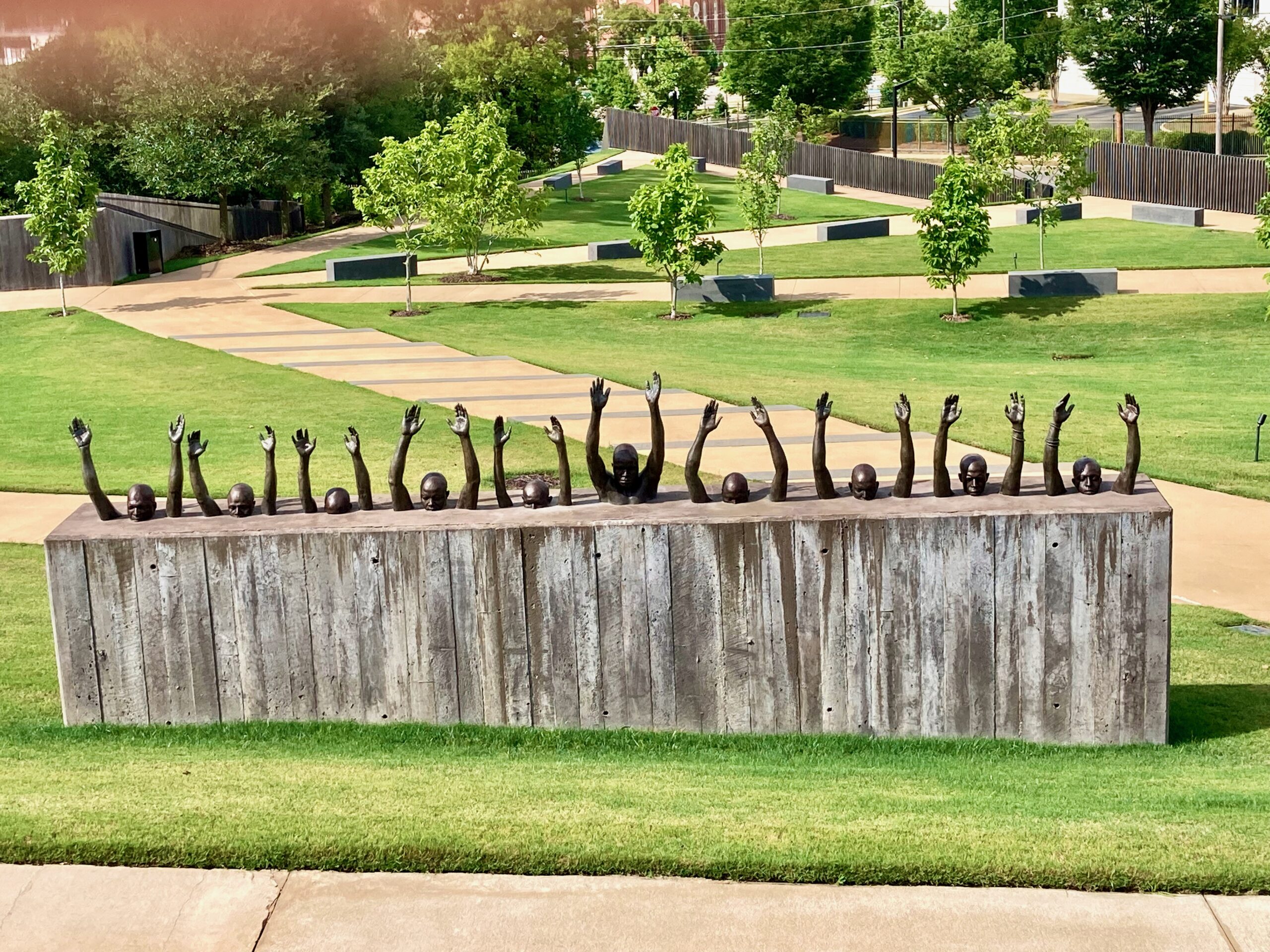
Relearning American History: A Self-Guided Tour of the South
July 7, 2021

Racism: A Global Pandemic
June 8, 2020
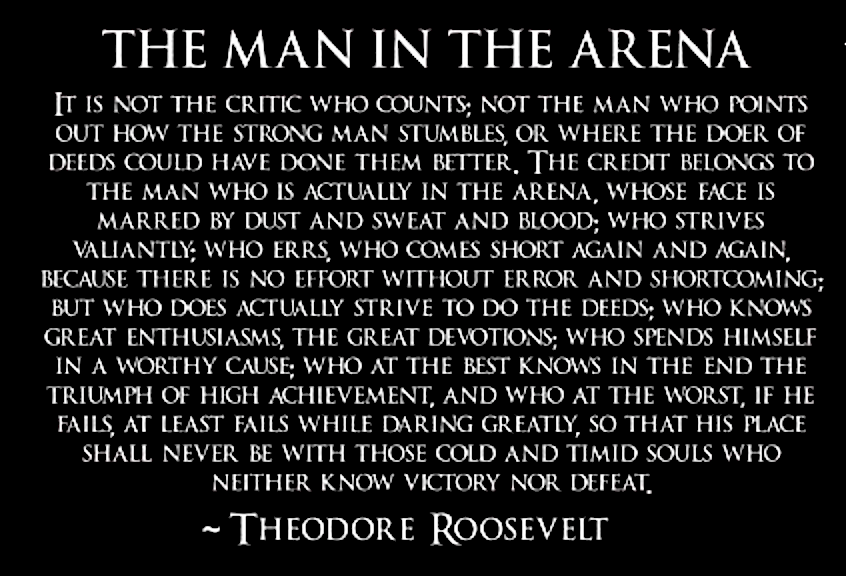
Daring Greatly
August 23, 2019

Becoming a Better Me
January 10, 2019